
This post, which was originally published at The Conversation, was written by Kevin Van den Wymelenberg, Leslie Dietz, and Mark Fretz.
Architects and building engineers strive to create safe, productive places where humans can live and work. We have developed complex codes, regulations, and guidelines to achieve goals such as structural safety, fire safety, adequate ventilation and energy efficiency, and to anticipate extreme scenarios such as 100-year floods. The question for our profession now is whether and how the 100-year viral pandemic will change architectural design and building operations.
How can societies safeguard buildings or homes from a viral pathogen during an epidemic? What would it take to redesign public and institutional buildings so they could help “flatten the curve,” instead of simply evacuating occupants? What if people could shape and modify the microbial communities present inside buildings to minimize exposure to harmful pathogens?
At the University of Oregon’s Biology and the Built Environment (BioBE) Center, we study interactions between humans, buildings, and microorganisms. We believe that architecture needs to adapt and evolve in ways that help people manage indoor microbiomes to support health. In a new paper, we combine research on how microbes function indoors with knowledge about the novel coronavirus to outline ways of minimizing COVID-19 transmission in buildings.
Cultivating or murdering microbes
Even in good times, and certainly during pandemics, the main thing people typically want to know about microbes is how to kill them. But in fact, the vast majority of microbes help humans more than they hurt us. The idea that microbes around us play an important role in our lives is known as the Old Friends Hypothesis or the Hygiene Hypothesis.
Each of us has our own microbiome—a collection of bacteria, fungi, viruses, and protozoa that inhabit our skin and body, and may be as unique as our fingerprints. Some of these microbes help keep us healthy, while others may cause us to become ill.
These organisms help regulate our digestion and impact our mood and our weight. Skin microbes can have immunoprotective effects.
There are also surprisingly complex microbial ecosystems within indoor spaces. Removing all microbial life from these settings can create problems. For example, irritable bowel disease, asthma, and some mood disorders have been linked to overall decreases in our microbial exposure. Lack of exposure during childhood is thought to spark over-reactive immune function later in life, potentially leading to increased inflammation and contributing to these afflictions.
Focusing solely on murdering microbes can have unintended consequences. For example, our lab recently discovered a correlation between concentrations of antimicrobial compounds and abundance of antibiotic-resistant bacteria indoors.
This finding has led our team to reexamine indoor cleaning practices more broadly.
Designing indoor microbiomes
Architects can use many design features to shape and modify microbial communities within homes and office buildings. They include space configuration and occupant density; interior material selection; window location, size and glass type; electric lighting spectrum and intensity; and air movement and ventilation strategies.
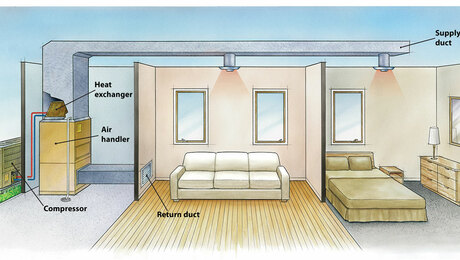
Building managers also play a role. They can adjust the amount of outside air that is admitted and the frequency at which it is exchanged with indoor air. Other levers include humidification and dehumidification, and of course, cleaning products and practices.
Our recent research suggests that many natural systems, such as daylight and natural ventilation, don’t just reduce energy consumption and support human health, they also support more diverse indoor microbial ecosystems and reduce the abundance of potential pathogens. Similarly, natural unfinished wood surfaces have been shown to reduce the abundance of some viruses more quickly than other common indoor surfaces, such as stainless steel or plastic.
Humidification is an important influence in indoor settings. Most indoor environments are very dry in the heating season. Dampness can produce mold, but very dry air is also a problem. It dehydrates our mucus membranes and skin and carries particles deeper into our respiratory tract, leaving us more susceptible to infection.
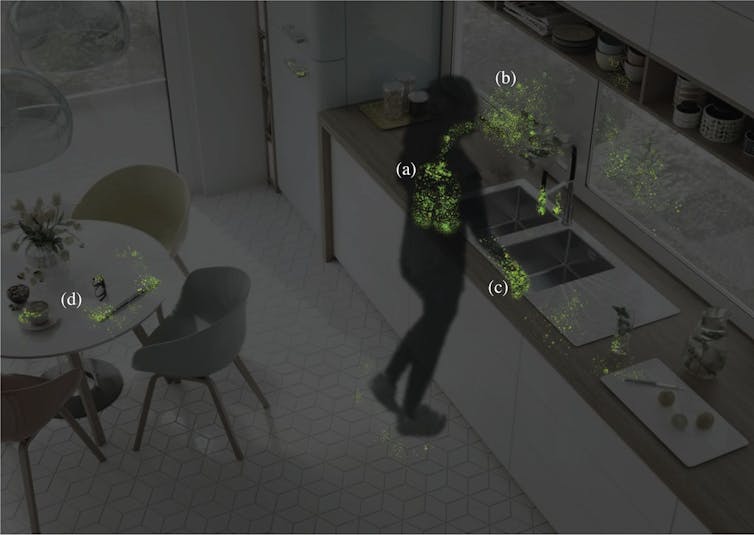
Dry air also decreases particle deposition, allowing ultra-fine particles to remain aerosolized longer. This increases the risk of airborne transmission of microbes.
Indoor air with a relative humidity of 40%-60% avoids these harmful impacts. It has also been shown to decrease viral infectivity, likely by disrupting viruses’ outer membrane
Based upon our past research, we have developed some basic guidelines for enhanced building operations during the COVID-19 pandemic. They aim to reduce the risk of indoor viral transmission in settings including homes, medical buildings, and other critical infrastructure.
These strategies can be applied in nearly every building. Examples include introducing more outside air, increasing air exchange, maintaining relative humidity of 40%-60%, opening windows to provide natural ventilation and flush out indoor spaces, increasing access to daylight, and implementing targeted disinfection techniques, such as UV-C light in health care settings.
People can use similar strategies to reduce risks at home. If someone in the house has been infected or is symptomatic, we recommend having them self-isolate in a space next to a bathroom with an exhaust fan that can operate continuously. This will pull air from the rest of the home through the infected space and out the bathroom exhaust.
Letting in sunlight and fresh air and maintaining healthy humidity levels can help create a healthy indoor environment at home during the COVID-19 pandemic.
Better living through microbiology
Our team’s next goal is to define what makes up a community of beneficial microbes. We are partnering with industry, institutions, and government organizations to develop real-time indoor microbial monitoring technologies that can support better operating practices and improve contact tracing strategies. With this knowledge, we can monitor for pathogens and use data science to improve our understanding of healthy indoor microbiomes.
How might people cultivate an indoor community of benign and favorable microbes? Several cleaning product manufacturers are already exploring the idea of adding specific microbes to indoor environments to outcompete or attack harmful microbes and curate others. These products avert many traditional cleaners’ “scorched Earth” approach, which relies on caustic and volatile ingredients.
We believe this concept is worth exploring but should be based on robust research with effective oversight. The key agency in this area is the Environmental Protection Agency, which regulates antimicrobial products designed as pesticides, including cleaning products.
For several decades, the architectural design and construction industry has been developing standards to guide building performance, including aspects related to human health. In our view, it is time to focus on shaping healthy indoor microbiomes so that they can shape us.
–Kevin Van den Wymelenberg, is Associate Professor of Architecture and Director, Biology and the Built Environment Center, University of Oregon; Leslie Dietz is Wet Lab Manager, University of Oregon; and Mark Fretz is Research Assistant Professor of Architecture, University of Oregon.
Weekly Newsletter
Get building science and energy efficiency advice, plus special offers, in your inbox.














5 Comments
> we recommend having them self-isolate in a space next to a bathroom with an exhaust fan that can operate continuously.
That should be "open to a bathroom". If that isn't possible, then add a low CFM window fan (blowing outward).
Also consider the reverse case - one healthy but high risk person and others of unknown status. Then you want the room for the former pressurized with outside air (eg, window fan blowing inward).
Perhaps a good number of COVID19 fatalities would have been avoided with more of these techniques.
Clearly continuous exhaust ventilation in the "sick room" is the best approach to keeping airborne viruses from finding other hosts. The nearby bathroom ventilation approach might even put others at some slightly elevated risk unless the sick or infected person has exclusive use of that bathroom, but at a high ventilation rate the transfer risk appears to be pretty low.
There has been some evidence that suggests higher relative humidity in the air kills off the COVID19 virus on surfaces pretty quickly, but I wouldn't take that to the bank just yet. There has been more than enough disinformation and partial-truths on this topic being spread around already.
During the 1918 influenza pandemic it was discovered that high ventilation rates (leaving the windows open 24/7) made the contagion rates within a house or hospital was reduced. This led to a practice of extreme oversizing of heating systems in the 1920s to be able to accommodate extreme ventilation heating loads.
In turn that led to comfort problems with primarily steam, but also hydronic heating systems, which would overshoot the thermostat set points by quite a bit, followed by the slow heat decay of heat rate from the radiators as the thermal mass cools. But for every "solution problem" there is yet another "solution problem".
The use of silvery or golden-bronze low emissivity paint for radiators became commonplace in the 1920s, reducing the heat output of the radiators by 15-20%, and the invention of air-restrictive radiator covers to knock back the rate of convective heat transfer for another 10-30% reduction (depending on the cover). The reduced heat emittance of those took the edge off the "hot flash" temperature overshoot problem, but led to efficiency robbing boiler short-cycling and other issues with the heating systems, since the radiation is now undersized for the boiler's burner size.
Dana--awesome bringing that up. I learned this stuff reading (and seeing) Dan Holohan at HeatingHelp--if anyone else is interested in a deep dive: https://heatinghelp.com/blog/metal-paints-and-radiators/
Dana-
that's all very interesting.I remember my father who was born in 1925, at night would crank up the heat in the winter and open the windows, he said it was how he grew up and that it was healthier, but never explained why. It was the Spanish flu. A lot of the homes we have worked on in New Haven CT built in the 1920's or later have giant radiators and giant double hung windows. I knew it was so they could keep the windows open in the winter for "health" but i never knew exactly what the background was on that. Can you imagine the level of air pollution back then when everyone heated with coal fired steam boilers running full tilt all winter so they could keep some windows open. The sky must have been gray all winter long with coal smoke. Probably very high rates of long cancer back then even for the very small portion of the population that did not smoke. Interesting stuff to consider. We have it much better now.
>"Can you imagine the level of air pollution back then when everyone heated with coal fired steam boilers running full tilt all winter so they could keep some windows open."
Coal fired boilers were another explicit reason (going back to at least the 1890s, maybe earlier) to put radiators by the windows and keep them cracked open. Ventilation lowered the risk of death by carbon monoxide poisoning.
As late as the 1950s coal was the primary space heating fuel in the UK, but that began to change in the decades following London's killer fog event in 1952, responsible for over 10,000 deaths in the course of a week or so. The atmospheric chemistry that made that week more lethal than "normal" smog wasn't well understood until much later, but coal burning was implicated as a primary factor early on. There is a fair amount of newsreel footage showing just how dark it was at mid-day during that event available on the web.
Log in or create an account to post a comment.
Sign up Log in